What Does a PTSD Episode Look Like? (Internal Feelings vs. External Signs)
January 30, 2026 | By Camila Jensen
When people ask, "what does a ptsd episode look like?" they often imagine dramatic scenes from movies: a soldier diving for cover when a car backfires or someone screaming during a nightmare. While these reactions happen, the reality of Post-Traumatic Stress Disorder is often much quieter, more complex, and deeply confusing for both the person experiencing it and their loved ones.
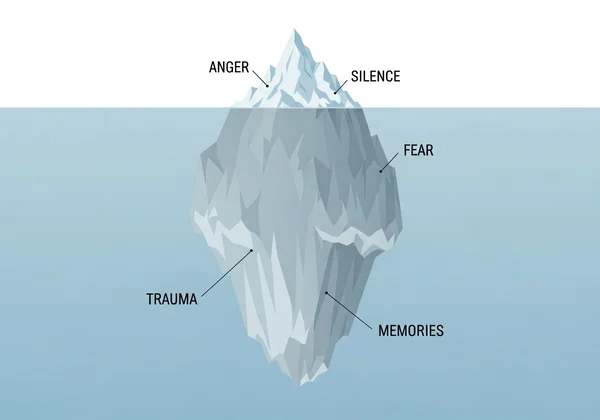
Think of a PTSD episode like an iceberg. The part visible above the water—the irritability, the silence, or the shaking—is just a small fraction of the event. Beneath the surface, there is a massive, invisible storm of memories, physical pain, and emotional flooding. If you are unsure where your symptoms stand, you can explore the PCL-5 test online to gain a better understanding of your baseline.
This guide explores that hidden depth. Whether you are trying to understand your own reactions or decode the behavior of someone you love, we will break down exactly what an episode looks like from the outside and, more importantly, what it feels like on the inside.
The External View: What It Looks Like to Others
For friends, partners, and family members, witnessing a loved one’s episode can be frightening. You might feel like you are walking on eggshells, unsure of what triggered the change.
When you search for what does a PTSD episode look like to others, you are usually looking for explanations for sudden behavioral shifts. The signs often fall into two distinct categories based on how the nervous system is reacting: the "Fight" response or the "Freeze" response.
The "Fight" Response: Outbursts and Sudden Irritability
Sometimes, the nervous system detects a threat that isn't there, sending the body into high-alert mode. To an observer, this doesn't look like fear; it looks like anger.
- Sudden Rage: A small inconvenience, like a dropped set of keys, might trigger a disproportionate explosion of anger.
- Aggressive Body Language: Clenched fists, a rigid jaw, or pacing back and forth.
- Defensiveness: Interpreting neutral comments as attacks or criticism.
The "Freeze" Response: The "Thousand-Yard Stare" & Zoning Out
On the other end of the spectrum, the body might decide that the safest option is to shut down. This is often confused with being ignored or being "moody."
- The Thousand-Yard Stare: The person’s eyes may look glassy or unfocused. They might look through you rather than at you.
- Non-Responsiveness: You might ask a question three times and get no answer.
- Physical Collapse: They may slump in a chair, curl up in bed, or seem unable to move their limbs (heaviness).
Physical Indicators: Trembling, Sweating, and Agitation
Even if the person tries to hide their emotional state, their body often reveals the truth. Physical signs of a PTSD episode can include:
- Visible trembling or shaking hands.
- Pale or flushed skin.
- Rapid, shallow breathing (hyperventilation).
- Excessive sweating, even in a cool room.
- An exaggerated "startle response" (jumping violently at sudden noises).
The Internal Experience: What It Feels Like
If you are the one going through it, the question isn't "what does it look like?" but rather "why does it feel like I'm dying?"
Understanding what does a PTSD episode feel like requires acknowledging that your body is reacting to a past event as if it is happening right now. The brain’s timekeeper breaks down, and the past bleeds into the present.
Reliving the Trauma: Intrusive Memories and Sensory Overload
This is not just "remembering" a bad event. It is a full-body re-experience.
- Flashbacks: You might see images overlaying your current reality.
- Auditory Intrusions: You might hear specific sounds (screams, crashes, voices) associated with the trauma.
- Olfactory Hallucinations: Smelling smoke, cologne, or other scents linked to the event is very common and can be incredibly disorienting.
Somatic Symptoms: Racing Heart, Nausea, and "Body Memories"
Often, the body remembers what the mind tries to forget. You might experience physical pain or sensations without a clear memory attached. This creates a terrifying sense of losing control.
Common internal sensations include:
- Chest tightness that mimics a heart attack.
- Severe nausea or "knots" in the stomach.
- A sensation of heat or cold flooding the body.
- Numbness or tingling in extremities.
Time Distortion & Dissociation: Losing Track of Reality
During an episode, time can feel elastic. Five minutes might feel like five hours, or you might lose hours of time completely.
This is often linked to dissociation—a feeling of being detached from your body. You might feel like a robot, or like you are watching yourself from across the room. The world around you might look "fake," two-dimensional, or foggy.
Mini-Checklist: Do These Sensations Sound Familiar?
- Do sudden noises make your heart race instantly?
- Do you sometimes feel like you are "watching a movie" of your life rather than living it?
- Do you have physical pain (like backaches or headaches) that doctors can't explain?
- Do you feel an intense need to escape crowded places immediately?
Note: Recognizing these signs is a form of self-awareness, not a diagnosis. If this checklist resonates with you, it may be helpful to explore our PCL-5 online test to gain deeper clarity.

Distinguishing the Episodes: Flashback vs. Panic Attack
One of the most common sources of confusion is distinguishing between a standard panic attack and a PTSD-related episode. While they share physical symptoms (racing heart, sweating, fear), the root cause is different.
The Key Difference: The Role of Past Memory
A panic attack is generally a fear of the immediate future or a fear of the symptoms themselves (e.g., "I am going to die," "I am going crazy"). It is often anxiety about what might happen.
A PTSD flashback, however, is anchored in the past. It is a reaction to something that did happen. During a flashback, you aren't just afraid; you are essentially time-traveling back to the traumatic moment.
Visual vs. Emotional Flashbacks (Common in C-PTSD)
Not all flashbacks involve seeing images. In Complex PTSD (C-PTSD), people often experience Emotional Flashbacks.
In an emotional flashback, you may not have a visual memory of the trauma. Instead, you are suddenly overwhelmed by the intense feelings you felt during the trauma—such as feeling small, helpless, ashamed, or terrified—without knowing why. You might revert to feeling like a frightened child, even if you are a competent adult in a safe environment.
The "Emotional Hangover": What Happens After an Episode
The episode doesn't end when the shaking stops. When you search for what happens after a PTSD episode, you are likely looking for validation for the exhaustion you feel.
The Physical Crash: Exhaustion and Fatigue
Adrenaline is a high-energy resource. When your body dumps adrenaline into your system for 20 minutes (or two hours) to fight a perceived threat, the crash is severe.
- You may need to sleep for several hours or days.
- Your muscles may be sore from tension.
- Your brain may feel "foggy" or slow.
The "Vulnerability Hangover": Shame and Guilt
Perhaps the most painful part of the aftermath is the shame. If you had an outburst, you might feel guilty about yelling at a loved one. If you froze/shut down, you might feel weak or embarrassed.
This "shame spiral" can sometimes trigger a secondary wave of anxiety, creating a vicious cycle. It is vital to remember: This is biology, not a character flaw.
Moving From Uncertainty to Clarity (The PCL-5 Screening)
Reading about symptoms can sometimes be overwhelming. You might see yourself in some of these descriptions but feel unsure about others. You might wonder, "Is this really PTSD, or am I just stressed?"
It is normal to seek concrete answers. Validating your experience is often the first step toward regaining control.
Why Validating Your Experience Matters
Living with undiagnosed symptoms is exhausting. It requires constant energy to mask your feelings and "act normal." Giving your experience a name—or at least understanding its severity—can lift a massive weight off your shoulders. It shifts the narrative from "What is wrong with me?" to "What happened to me?"
How the PCL-5 Tool Helps You Understand Your Patterns
The PCL-5 (Posttraumatic Stress Disorder Checklist for DSM-5) is the gold-standard tool used by professionals to assess symptom severity. It doesn't just give you a label; it helps categorize your experiences into four key areas:
- Intrusions (Unwanted memories)
- Avoidance (Staying away from reminders)
- Negative alterations in cognition/mood (Guilt, shame)
- Alterations in arousal (Hypervigilance)
Confidential & Educational: Take the Free Assessment
We offer a secure, confidential way to screen your symptoms using official criteria. This is not a medical diagnosis, but an educational resource to help you see the full picture of your mental health.
By completing the assessment, you can receive an optional AI-driven report that breaks down your specific symptom profile and offers actionable next steps.
Start My Confidential Assessment
Immediate Response: What to Do During an Episode
Whether you are the one experiencing the episode or the one witnessing it, having a plan is essential. Here are immediate steps to take when the storm hits.
Grounding Techniques to Anchor Yourself
If you feel yourself slipping into a flashback or dissociation, try the 5-4-3-2-1 Method to bring your brain back to the present moment:
- 5 things you can see.
- 4 things you can physically feel (the fabric of your chair, your feet on the floor).
- 3 things you can hear.
- 2 things you can smell.
- 1 thing you can taste.
How to Support a Loved One (Do's and Don'ts)
- DO use a calm, low voice.
- DO ask simple questions: "You are safe here. Can you feel your feet on the floor?"
- DON'T touch them without asking (touch can be a trigger).
- DON'T shout or demand they "snap out of it."
- DON'T try to rationalize with them until the episode is over.
Safety Check: When to Seek Immediate Emergency Help
While most episodes resolve on their own with time and grounding, safety is the priority. You should seek immediate emergency help (call 911 or a crisis line) if:
-
The person threatens to harm themselves or others.
-
The person is experiencing a psychotic break (hallucinations not related to memory).
-
The dissociation is so severe they are wandering into unsafe situations (traffic, etc.).

Understanding is the First Step Toward Healing
Recognizing what a PTSD episode looks like strips away the fear of the unknown. These episodes are not signs of madness; they are the result of a brain that is trying desperately to survive.
If you recognized yourself or a loved one in these descriptions, know that you are not broken. You are dealing with a distinct, manageable condition. Knowledge is your most powerful tool. Whether you choose to check your traits with this PCL-5 test or speak to a therapist, taking action is an act of courage.
Frequently Asked Questions About PTSD Episodes
How long does a PTSD episode usually last?
The duration varies significantly. A specific flashback might last only a few minutes, while the resulting high-anxiety state or emotional "flare-up" can last for hours or even days.
Can you have a PTSD episode without a clear trigger?
Yes. While external triggers (sounds, smells) are common, internal triggers (emotions, heart rate changes) or subconscious associations can launch an episode without warning.
Is it safe to wake someone up from a PTSD nightmare?
Proceed with caution. Waking someone suddenly can trigger a violent "startle response." It is safer to use your voice from a distance to gently wake them rather than shaking or touching them.
Why do people with PTSD push loved ones away during an episode?
This is often a protective mechanism. They may feel overwhelmed and unable to process social interaction, or they may fear hurting you with their outburst. Isolation feels safer to an overloaded nervous system.
Can a PTSD episode cause physical pain?
Yes. The intense muscle tension, hormonal spikes, and "body memories" associated with trauma can cause migraines, back pain, stomach cramps, and generalized body aches.